When to Ask for a Heart Screening: A Guide for Women
Last updated: February 6, 2026
Heart disease remains the leading cause of death for women in the United States, yet many women remain unaware of when they should begin heart screenings or what tests they actually need. The approach to heart screening women receive should be tailored to their unique risk factors and life stages, but confusion about timing often leaves women vulnerable to undetected cardiovascular issues.
At Ms. Medicine, we believe that understanding your cardiovascular risk helps determine screening frequency and ensures you receive the personalized care you need to protect your heart health.
Women are 50% more likely than men to receive an incorrect initial diagnosis following a heart attack. This disparity stems partly from the fact that women’s heart disease symptoms often differ from men’s, and screening protocols haven’t always accounted for these differences. Regular heart screenings for women can detect issues early, but only when the timing and tests are appropriate for each woman.
Why Heart Screening for Women Differs from Men
Women face unique cardiovascular challenges that make personalized screening essential. Hormonal changes throughout a woman’s life significantly impact heart health, from pregnancy-related conditions like preeclampsia to the cardiovascular effects of menopause. These factors mean that heart screening for women requires consideration of more than just age and family history.
Traditional cardiovascular risk calculators were developed primarily using data from men, leading to an underestimation of risk in women. Women are more likely to develop heart disease in smaller blood vessels, a condition called microvascular disease, which standard stress tests might miss. Additionally, conditions like autoimmune diseases, which affect women disproportionately, can increase cardiovascular risk in ways that standard screening protocols don’t always capture.
Ms.Medicine providers understand these nuances. Our women-focused approach ensures your cardiovascular risk assessment accounts for factors that specifically affect women’s heart health, not just the traditional risk factors developed for men.
Heart Screening Timeline: When to Start and What to Expect
Ages 20-39: Establishing Your Baseline
Your twenties and thirties are the ideal time to establish baseline heart health measurements. During your annual preventive health checkup, basic cardiovascular screening should include blood pressure monitoring, cholesterol testing, and assessment of lifestyle factors.
Women should have their first cholesterol screening by age 20, or earlier if they have risk factors like family history of early heart disease, diabetes, or high blood pressure. Blood pressure should be checked at least every two years if it’s normal, or more frequently if elevated.
This is also the time to discuss any pregnancy-related cardiovascular complications with your provider. Conditions like gestational diabetes, preeclampsia, or pregnancy-induced high blood pressure can increase your long-term cardiovascular risk and may warrant earlier or more frequent screening.
Ages 40-49: Intensifying Surveillance
As women enter their forties, cardiovascular risk begins to increase, making this decade crucial for more intensive screening. A thorough preventive health checkup should now include annual cholesterol testing and blood pressure monitoring at every healthcare visit.
This is when many women should consider their first electrocardiogram (EKG) to establish a baseline reading of their heart’s electrical activity. If you have risk factors like diabetes, high blood pressure, or a strong family history of heart disease, your provider might recommend additional tests like a stress test or coronary calcium scoring.
Women approaching menopause should pay particular attention to cardiovascular health, as declining estrogen levels can affect cholesterol levels and blood vessel function. Understanding your cardiovascular risk during this transition helps determine whether you need more frequent monitoring or preventive interventions.
Ages 50 and Beyond: Comprehensive Assessment
After menopause, women’s cardiovascular risk increases significantly, making comprehensive screening essential. Annual cholesterol testing becomes standard, along with regular blood pressure monitoring and diabetes screening.
Many women in this age group benefit from coronary calcium scoring, a specialized CT scan that measures calcium buildup in the coronary arteries. This test provides valuable information on cardiovascular risk that traditional risk calculators may miss, particularly in women.
Depending on your risk factors, your provider might recommend stress testing, echocardiograms, or other specialized cardiac imaging. The key is working with a provider who understands how to interpret these tests in the context of women’s unique cardiovascular risk profile.
Understanding Different Types of Heart Screenings
Basic Screening Tests
Blood pressure measurement remains the most fundamental cardiovascular screening tool. However, it’s important to ensure accurate readings by using the proper cuff size and technique, as women’s arms are often smaller than the standard cuff accommodates.
Cholesterol testing should include a complete lipid panel measuring total cholesterol, LDL (bad) cholesterol, HDL (good) cholesterol, and triglycerides. Women’s cholesterol levels fluctuate more than men’s due to hormonal changes, so the timing of testing and interpretation of results requires expertise in women’s health.
Advanced Screening Options
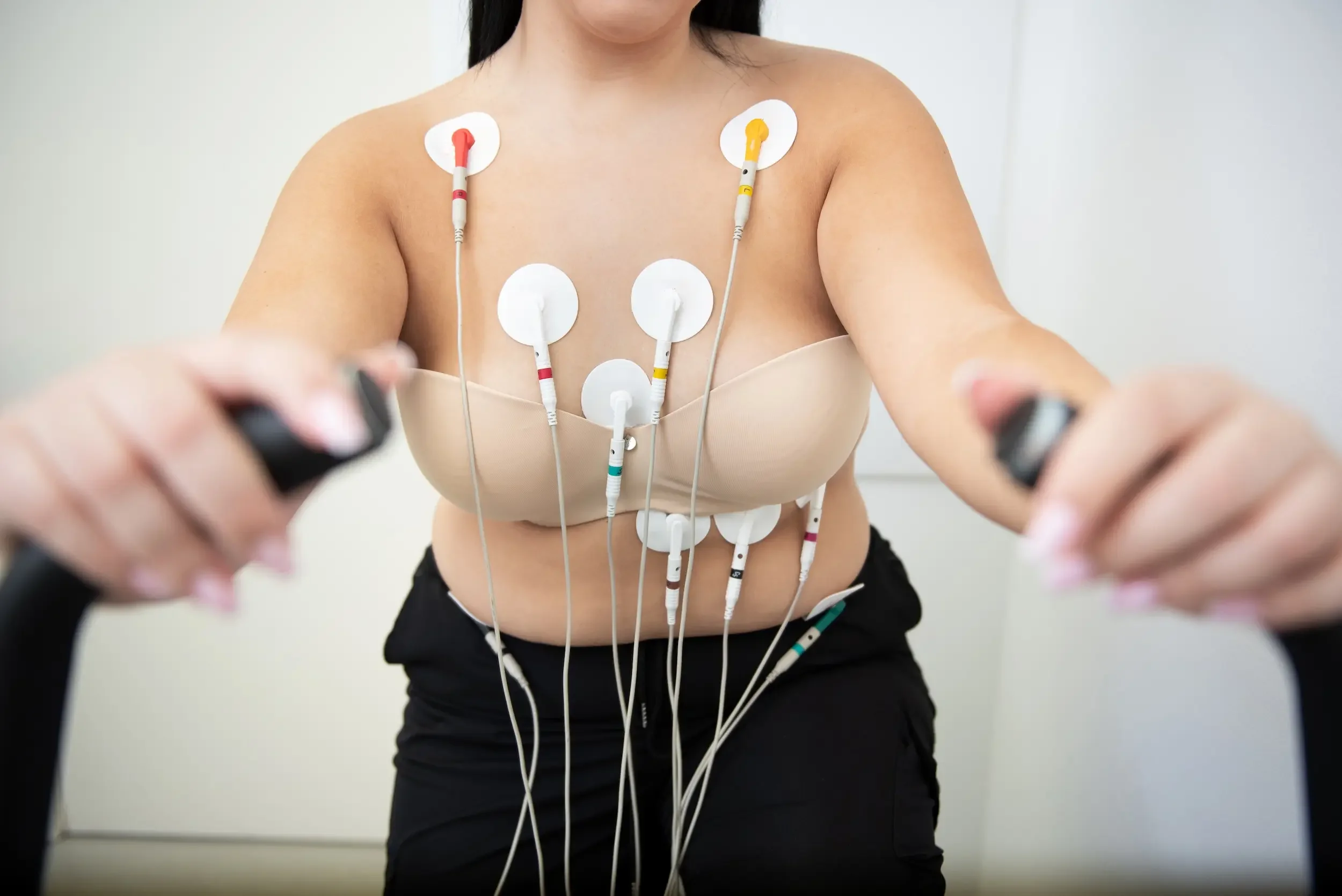
Electrocardiograms (EKGs) provide a snapshot of your heart’s electrical activity and can detect irregular rhythms or signs of previous heart damage. While a single EKG might not reveal intermittent problems, it establishes a baseline for comparison in future tests.
Stress testing evaluates how your heart responds to increased demand, either through exercise or medication. For women, exercise stress testing is often preferred when possible, as it provides more accurate results than pharmacological stress testing.
Coronary calcium scoring uses CT technology to measure calcium deposits in coronary arteries, providing insight into atherosclerosis progression. This test is particularly valuable for women whose traditional risk factors might not fully capture their cardiovascular risk.
Specialized Testing for Women
Echocardiograms use ultrasound to evaluate heart structure and function and can detect conditions such as heart valve problems or cardiomyopathy that might be missed by other tests. Women are more likely than men to develop certain types of heart muscle disease, making this test particularly valuable.
For women with symptoms like chest pain or shortness of breath, specialized testing might include cardiac MRI or nuclear stress testing, which can detect microvascular disease that affects women more frequently than men.
Women-Specific Risk Factors That Affect Screening Timing
Pregnancy-Related Complications
Women who experienced preeclampsia, gestational diabetes, or pregnancy-induced high blood pressure have increased cardiovascular risk that persists long after pregnancy. These women should begin more intensive screening earlier and maintain closer monitoring throughout their lives.
Pregnancy complications can double a woman’s risk of developing heart disease later in life, yet many women and their providers don’t connect these pregnancy experiences to future cardiovascular health. At Ms.Medicine, we ensure your complete health history informs your screening recommendations.
Autoimmune Conditions
Conditions like rheumatoid arthritis, lupus, and other autoimmune diseases significantly increase cardiovascular risk in women. The chronic inflammation associated with these conditions accelerates atherosclerosis, often requiring earlier and more frequent heart screening.
Women with autoimmune conditions should work with providers who understand the link between inflammation and cardiovascular risk, and ensure screening protocols account for this increased risk.
Hormonal Factors
Early menopause, whether natural or surgical, increases cardiovascular risk and may warrant earlier screening. Similarly, women who used certain types of hormone replacement therapy or birth control pills may have different risk profiles that affect screening recommendations.
PCOS (polycystic ovary syndrome) affects up to 10% of women of reproductive age and significantly increases cardiovascular risk through its effects on insulin resistance, blood pressure, and cholesterol levels.
Taking Control of Your Heart Health Journey
Understanding when to request a heart screening and which tests you need empowers you to advocate for appropriate care and catch potential problems early.
At Ms.Medicine, we’ve reimagined the healthcare experience to prioritize your individual needs and risk factors. Our concierge care model means you’ll have time to discuss your cardiovascular risk factors thoroughly, understand your screening results completely, and develop a personalized prevention plan.
Don’t wait for symptoms to appear before taking your heart health seriously. Women’s heart disease often presents differently from men’s, and by the time symptoms develop, significant damage may have already occurred. Proactive screening based on your individual risk factors and life stage is your best defense against cardiovascular disease.
Download our free Heart Health Guide to learn more about protecting your cardiovascular health and understanding your personal risk factors.
Ms.Medicine providers are experts in women’s health, including the unique aspects of cardiovascular risk assessment and prevention in women. We’re here to help you navigate the confusion around screening timing and ensure you get the personalized care you deserve.
References and Additional Resources:
American Heart Association - Women and Heart Disease: https://www.goredforwomen.org/en/about-heart-disease-in-women
Centers for Disease Control and Prevention - Women’s Heart Disease Facts: https://www.cdc.gov/heart-disease/about/women-and-heart-disease.html
American College of Cardiology - Cardiovascular Disease in Women: https://www.acc.org/Latest-in-Cardiology/Articles/2023/04/01/01/42/Feature-Cardiovascular-Disease-in-Women-From-Maternal-Health-to-Menopause
Mayo Clinic - Heart Disease in Women: https://www.mayoclinic.org/diseases-conditions/heart-disease/in-depth/heart-disease/art-20046167
Harvard Health - Women’s Heart Health: https://www.health.harvard.edu/heart-health/the-five-factors-that-drive-heart-disease
WomenHeart - National Coalition for Women with Heart Disease: https://www.womenheart.org/